Blood pressure (hypertension / pre-HTN)
- Evidence: Recent umbrella/meta-analyses of RCTs report small BP reductions, with the clearest signal at ≥400 mg/day for ≥12 weeks (about −2–5 mmHg systolic/diastolic). Effects are larger in people with metabolic disease and smaller or absent in normotensive, magnesium-replete adults. PubMedPMCFrontiers
Takeaway: Modest BP benefit, most likely if you’re hypertensive or insulin-resistant and you take adequate doses long enough.
Type 2 diabetes / glycemic control
- Evidence: Meta-analyses of RCTs show lower fasting glucose after supplementation and little to modest change in HbA1c overall; some subgroup analyses suggest improvements in lipids (↑HDL) without consistent effects on LDL/TG. PMCPubMedNature
Takeaway: Helpful as an adjunct (especially if dietary magnesium is low); don’t expect large HbA1c shifts by itself.
Depression / mood
- Evidence: A 2023 meta-analysis of randomized trials found a significant reduction in depression scores with magnesium vs placebo (SMD ≈ −0.92). Authors call for larger, higher-quality RCTs, but the direction of effect is consistent. PMCPubMed
Takeaway: Promising, especially for mild–moderate symptoms; more large RCTs still needed.
Migraine prevention
- Evidence: Reviews and society resources support oral magnesium (often oxide/citrate 400–600 mg/day) as a reasonable preventive option; the RCT base is mixed but generally favorable. (Acute treatment evidence mainly supports IV magnesium, not oral.) American Migraine FoundationAmerican Headache SocietyPain Physician
Takeaway: Reasonable preventive adjunct with a good safety profile; dose commonly 400–600 mg/day (oxide or citrate).
Sleep / insomnia
- Evidence: Systematic reviews note mixed/uncertain effects; small RCTs (older adults, various forms including bisglycinate or threonate) show modest improvements in some sleep measures, but evidence quality is low–moderate and heterogeneous. PMCPubMedScienceDirect
Takeaway: Possible small benefit for subjective sleep quality; not a reliably proven insomnia treatment.
Chronic constipation
- Evidence: A 2019 double-blind RCT showed magnesium oxide improved stool frequency and transit time. In 2023, AGA/ACG guidelines gave conditional recommendations for magnesium oxide (low–very low certainty), alongside fiber and senna. PMCAmerican College of GastroenterologyAmerican Gastroenterological Association
Takeaway: Effective osmotic laxative option; evidence supports use, though guideline certainty is low.
Muscle cramps (idiopathic)
- Evidence: The Cochrane review (2020) concluded magnesium is unlikely to provide clinically meaningful prophylaxis for idiopathic leg cramps in older adults; pregnancy-associated cramps evidence is conflicting. Later reviews echo this. PubMedPMC
Takeaway: Not helpful for typical idiopathic leg cramps.
Inflammation markers
- Evidence: Findings are mixed. Some meta-analyses report CRP reductions with magnesium; others (including dose–response analyses) report no clear effect overall. PMCFrontiers
Takeaway: Possible anti-inflammatory effect, but not consistent across trials.
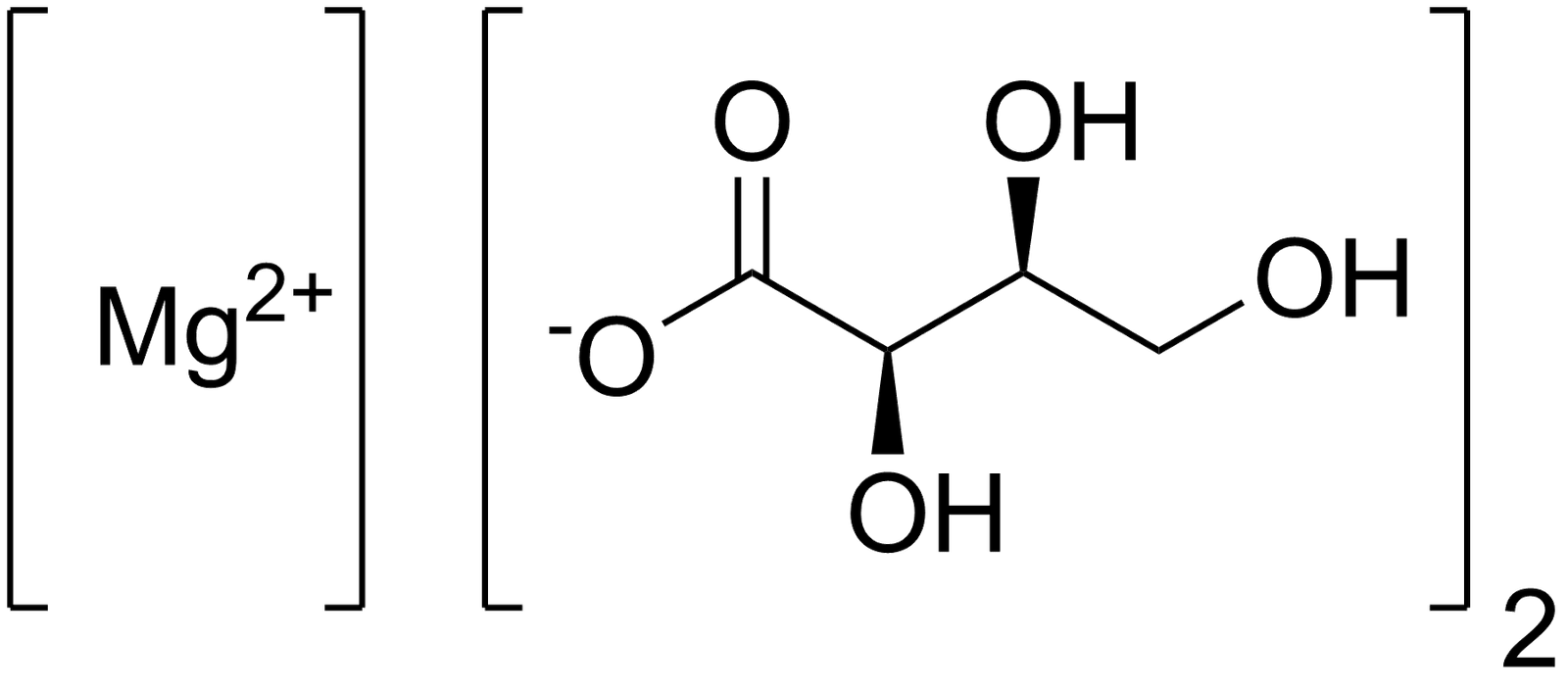
Forms & absorption (what matters for pills)
- Absorption varies by salt: citrate, lactate, chloride are generally more bioavailable than oxide/sulfate; products list elemental magnesium, not total compound weight. Office of Dietary Supplements
Safety, dosing, and interactions
- UL for supplements: The U.S. NIH lists a tolerable upper intake level (UL) of 350 mg/day from supplements (not counting food). Higher supplemental doses are commonly used short-term in trials and in constipation, but GI side effects (diarrhea, cramping) rise with dose. Kidney disease increases risk of hypermagnesemia. Office of Dietary Supplements
- Drug interactions: Separate magnesium from tetracycline/quinolone antibiotics and bisphosphonates (timing matters). Long-term PPIs can lower magnesium; clinicians sometimes monitor levels. Office of Dietary Supplements
Practical note: Many benefits in trials appear when deficiency or low intake is present. If you supplement, choose a well-absorbed form (e.g., glycinate or citrate) and start with lower elemental doses (100–200 mg/day) to tolerance. Discuss with a clinician if you have kidney issues or take interacting meds. Office of Dietary Supplements
Quick reference: representative studies/meta-analyses (2015–2025)
- Blood pressure: 2024 umbrella meta-analysis—BP reductions, strongest at ≥400 mg/day for ≥12 weeks. PubMed
- T2D glycemic control: 2025 and 2022–23 syntheses—↓ fasting glucose, minimal or small HbA1c changes. PubMedPMC
- Depression: 2023 RCT meta-analysis—lower depression scores vs placebo. PMC
- Migraine prophylaxis: Society resources + reviews support 400–600 mg/day oral magnesium as a preventive option (evidence mixed but favorable). American Migraine FoundationAmerican Headache Society
- Sleep: 2021 systematic review (older adults) + newer small RCTs—mixed/uncertain overall benefit. PMC
- Constipation: 2019 RCT (Mg oxide) + 2023 AGA/ACG guideline—conditional recommendation. PMCAmerican Gastroenterological Association
- Muscle cramps: 2020 Cochrane—unlikely to help idiopathic cramps. PubMed
- Inflammation: 2022 meta-analysis (↓CRP) vs 2022 dose-response (no effect)—inconsistent. PMCFrontiers